Headlines
April 19, 2024

CNN
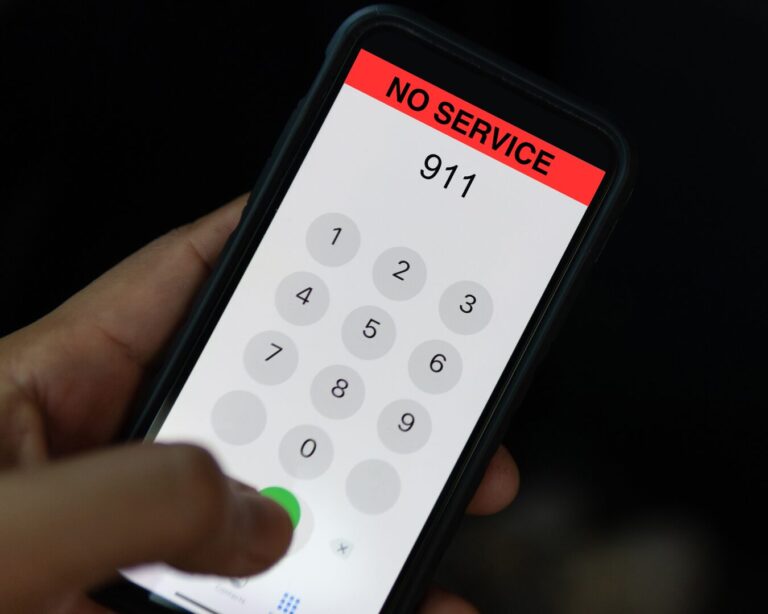
Meet the Trump Jurors
Twelve jurors and one alternate have been selected for Trump's hush money trial, comprising a diverse group with backgrounds ranging from sales and law to engineering and teaching.

CBS News
Taylor's Surprise, Double Album Drop
Taylor Swift announced "Fortnight" featuring Post Malone as the lead single from her eagerly awaited new album "The Tortured Poets Department," set for release at midnight EDT.

The Detroit News
Kennedy Makes Michigan Ballot
RFK Jr. has been named the Natural Law Party's presidential nominee in Michigan, providing him an official ballot position and giving the lesser-known party a prominent candidate for the election.

Columbia Daily Spectator
NYPD Comes to Columbia
Columbia University President Shafik authorized the NYPD to dismantle the "Gaza Solidarity Encampment," leading to over 100 arrests and the suspension of involved students.

Yahoo! Sports
Caitlin Clark Getting Her Own Shoe
Caitlin Clark is reportedly close to finalizing a lucrative eight-figure endorsement deal with Nike that includes her own signature shoe, significantly surpassing her WNBA salary.
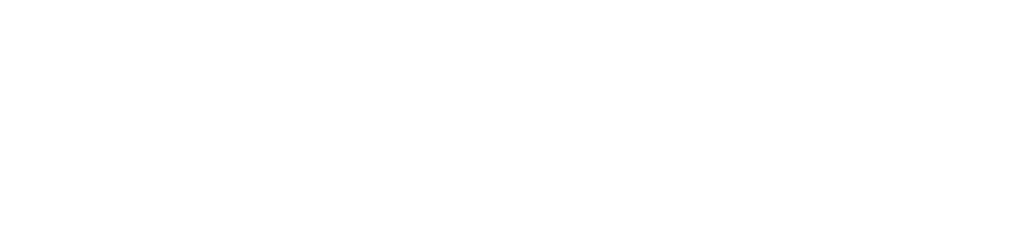
CNBC
Millions in U.S. Couldn't Call Police
Major 911 outages in Nebraska, South Dakota, Texas, and Nevada disrupted emergency communications until late Wednesday, potentially linked to increased cyber attack risks.
CNN
Why Is the Trump Jury Anonymous?
The jury for Trump's trial is anonymous to protect them from harassment and influence, reflecting a practice initially reserved for high-risk cases but now increasingly used in high-profile trials.

NPR
U.S. Tanks Palestinian Bid at U.N.
The US vetoed a UN Security Council resolution admitting the Palestinian Authority as a full member, maintaining that Palestinian statehood should follow a negotiated peace with Israel.
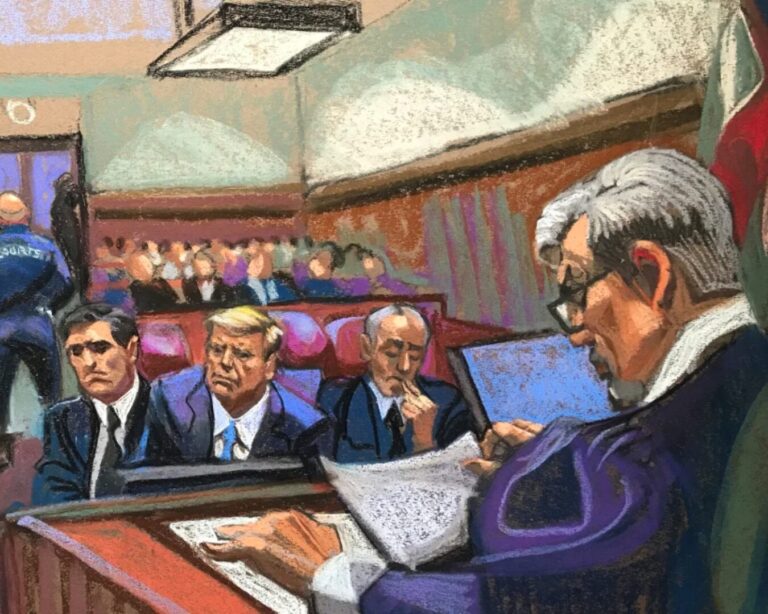
Forbes
'Dark Side of the Moon' Nears Milestone
Pink Floyd's "Dark Side of the Moon" is nearing a historic milestone as it approaches 1,000 weeks on the Billboard 200, boosted by a recent resurgence in interest linked to a solar eclipse.

NBC News
House Progressives Release Wish List
House progressives have released a 2025 agenda focusing on economic reforms and less on cultural issues, aiming to energize their base and influence President Biden's policies.

The Independent Florida Alligator
Florida Requires Teaching on Communism
DeSantis signed a bill that mandates education on the "dangers and evils of communism" in Florida public schools, starting in the 2026-27 school year, and includes the creation of a related museum.

6 ABC Philadelphia
Kennedy Family Supports Biden
During a campaign stop in Philadelphia, Biden received endorsements from over 15 Kennedy family members to counter the independent candidacy of RFK Jr., seen as a potential election spoiler.

USA Today
Remembering the Iconic Dickey Betts
Dickey Betts, a key member of The Allman Brothers Band, passed away, leaving behind a legacy of iconic songs like 'Ramblin' Man,' which he reflected on in previous interviews.
Deadline
Netflix Cracks Down on Passwords
Netflix Co-CEO Greg Peters reports that the crackdown on password sharing hasn't impacted viewership, supported by steady data and a subscriber increase partly due to the new policy.

National Bureau of Economic Research
Study: Incarceration and Immigration
A Study by NBER shows that for over 150 years, US immigrants have consistently had lower incarceration rates than the US-born, a gap that widened since 1960, unrelated to immigration policy.

The Hill
Johnson Advances Ukraine Aid
House conservatives, furious with Speaker Johnson for supporting a substantial Ukraine aid package, have yet to leverage their power to oust him, despite their vocal protests and threats.
BBC
Children Used as Guinea Pigs in Trial
Documents reveal that in the 1970s and 80s, UK children were subjected to medical trials with infected blood products, causing widespread hepatitis C and HIV infections among them.

RealClearPolitics
Salena: The Politics of U.S. Steel
The sale of US Steel to Nippon Steel, approved by shareholders but opposed by unions, politicians, and some executives, underscores concerns about the impact on workers and national interests.

The Guardian
Harry Now a U.S. Resident
Prince Harry has confirmed his U.S. residency four years after relocating to Southern California, further distancing himself from British royal duties and his role as a counselor of state.
For the Left
For the Right
Independent doesn’t mean indecisive.
© 2024 Smerconish. All rights reserved.
© 2024 Smerconish. All rights reserved.
News Links
Contact Links
Balance Delivered Daily
Get the Smerconish.com daily newsletter.
We will NEVER SELL YOUR DATA. By submitting this form, you are consenting to receive marketing emails from: Smerconish.com. You can revoke your consent to receive emails at any time by using the SafeUnsubscribe® link, found at the bottom of every email. Emails are serviced by Aweber
Privacy Policy | Website design by Creative MMS
Privacy Policy | Website design by Creative MMS