Headlines
March 7, 2026

Axios
Trump Demands “Unconditional Surrender”
President Trump told Axios Friday that his demand for Iran's "unconditional surrender" could mean the complete destruction of the regime's military capabilities — not necessarily a formal surrender.

NBC News
Russia Providing Intel to Iran
The assistance could help Iran locate American warships, radar or other communication systems, but there's no indication Moscow is helping direct Iranian strikes, sources tell NBC News.

Express
Iran Threatens To Nuke Israel
Iran has shared a chilling image of a nuclear missile striking an Israeli city, which appears to be Tel Aviv. In a post on X, the account previously belonging to Supreme Leader Ayatollah Ali Khamenei warned that "Khorramshahr is ahead"

NPR
84% of Republicans Support the War
As war with Iran heads toward a second week, most Americans say that they are against the military action and disapprove of how President Trump is handling it, according to the latest NPR/PBS News/Marist poll.

CBS News
Airstrikes Alone Can’t Change Regime
U.S. and Israeli airstrikes alone are unlikely to result in the ouster of the Iranian government, according to an expert in air campaigns, who said that the risks are growing for a more drawn-out war that could spread beyond the Middle East.

USA Today
Troop Complaints Over Religious Freedom
The United States' war in Iran has heightened existing concerns among some service members about the influence of Christian nationalism on the military under Pentagon chief Pete Hegseth's leadership.

The Wall Street Journal
Prediction Markets Drive College Frenzy
Prediction markets on college campuses are gaining popularity, enabling participants to trade contracts on event outcomes, though concerns about ethics and gambling risks persist.

The Washington Post
Don’t Imprison Parents for Their Kids
The guilty verdict Tuesday in the murder-by-proxy trial of a father whose son is accused of killing four people in a school shooting in Georgia sets a devastating and absurd precedent for imprisoning people for essentially being bad parents.

Variety
Ellison Vows CNN Independence
With David Ellison‘s media company poised to snap up CNN’s parent company, staffers at the news cable outlet have expressed fears that Paramount Skydance will steer CNN’s coverage toward a more conservative ideological bent.

Associated Press
Time To Debate Our Clocks Again
Even though polls show most people dislike the system that has most Americans changing clocks twice a year, the political moves necessary to change the system haven’t succeeded because opinions on the issue and its potential impacts are sharply divided.
ABC News
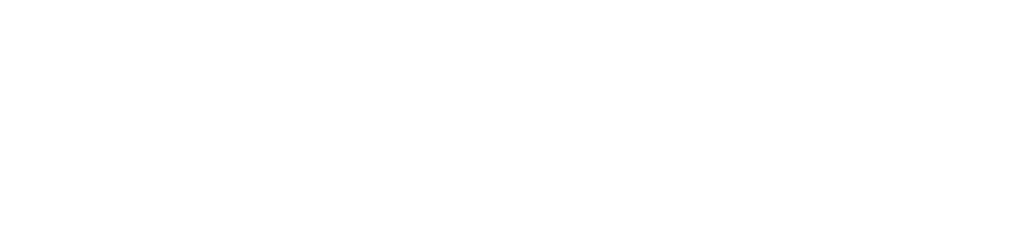
Files Released With Trump Claim
The Department of Justice on Thursday released three previously withheld FBI interview reports from 2019 related to a woman who made uncorroborated allegations that she was abused by Donald Trump in the 1980s, when she was a minor.

Politico
Dems Debate Whether To Spend in TX
Enthusiasm remains high for the party’s Senate nominee, James Talarico, but national Democrats aren’t sure how far they should go to support him — particularly if Sen. John Cornyn emerges from the GOP runoff in May.
The New York Times
Daryl Hannah: It Never Happened
Daryl Hannah explores the high-profile romantic relationship between her and John F. Kennedy Jr. in the early 1990s, highlighting the challenges they faced under media scrutiny and the impact on their personal and professional lives.

Barbara Fried
SBF Mom: “I’m Ending My Silence”
Sam Bankman-Fried’s mother argues for his innocence, criticizing the media’s "one-sided" portrayal and sensationalism. She highlights his 25-year sentence's personal toll and his commitment to the truth.
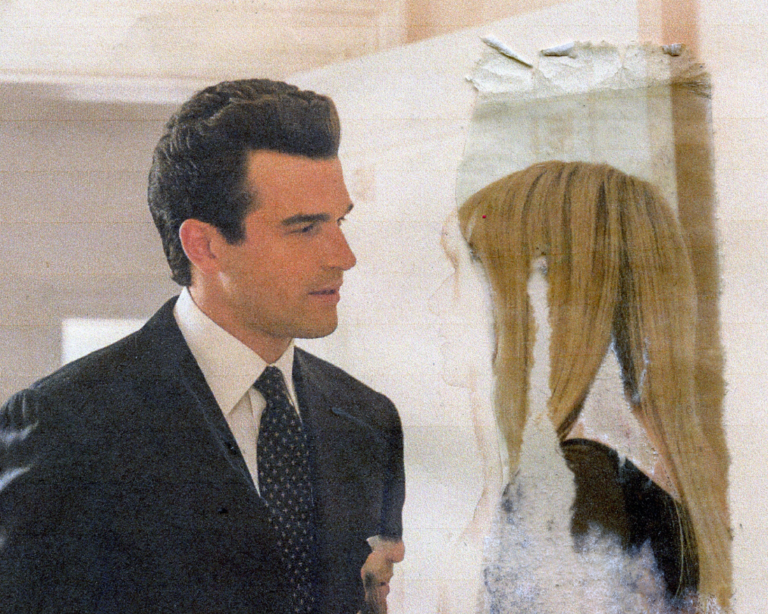
Mediaite
Obama Critiques Trump
Former President Barack Obama sounded off on President Donald Trump and his administration in a series of thinly-veiled attacks at Reverend Jesse Jackson’s funeral on Friday.

CNN
Trump Predicts Cuba’s Fall
“Cuba is gonna fall pretty soon, by the way, unrelated, but Cuba is gonna fall too. They want to make a deal so badly,” he told CNN’s Dana Bash in a phone interview when touting US military success in his second term.

CNBC
Jobs Growth Slows in February
Nonfarm payrolls in February fell by 92,000, compared with the estimate for 50,000 and below the downwardly revised January total of 126,000. It was the third time in five months that the economy lost jobs.

New York Post
Real Reason Noem Stayed Married
Bryon Noem‘s family members are hoping he finally leaves his wife, Kristi Noem, after the ultimate “humiliation” from her alleged affair with a top adviser — but fear he’ll continue to stay in his marriage.

The Hollywood Reporter
TFCA Resignations Over Censorship
The Toronto Film Critics Association faced a mass resignation after a pro-Palestine speech was censored, sparking debates on freedom of expression and the role of political discourse in artistic communities.
For the Left
For the Right
Independent doesn’t mean indecisive.